Mammogram Data Annotation for AI-Driven Breast Cancer Detection
Mammographic screenings are widely known for their accessibility, cost-efficiency, and dependable accuracy in detecting abnormalities. However, with over 100 million mammograms taken globally each year, each requiring at least two specialist reviews—the sheer volume creates significant challenges for radiologists, leading to delays in report generation, missed screenings, and an increased risk of diagnostic errors. A… Continue reading Mammogram Data Annotation for AI-Driven Breast Cancer Detection The post Mammogram Data Annotation for AI-Driven Breast Cancer Detection appeared first on Cogitotech.

Mammographic screenings are widely known for their accessibility, cost-efficiency, and dependable accuracy in detecting abnormalities. However, with over 100 million mammograms taken globally each year, each requiring at least two specialist reviews—the sheer volume creates significant challenges for radiologists, leading to delays in report generation, missed screenings, and an increased risk of diagnostic errors. A study by the National Cancer Institute suggests screening mammograms underdiagnose about 20% of breast cancers.
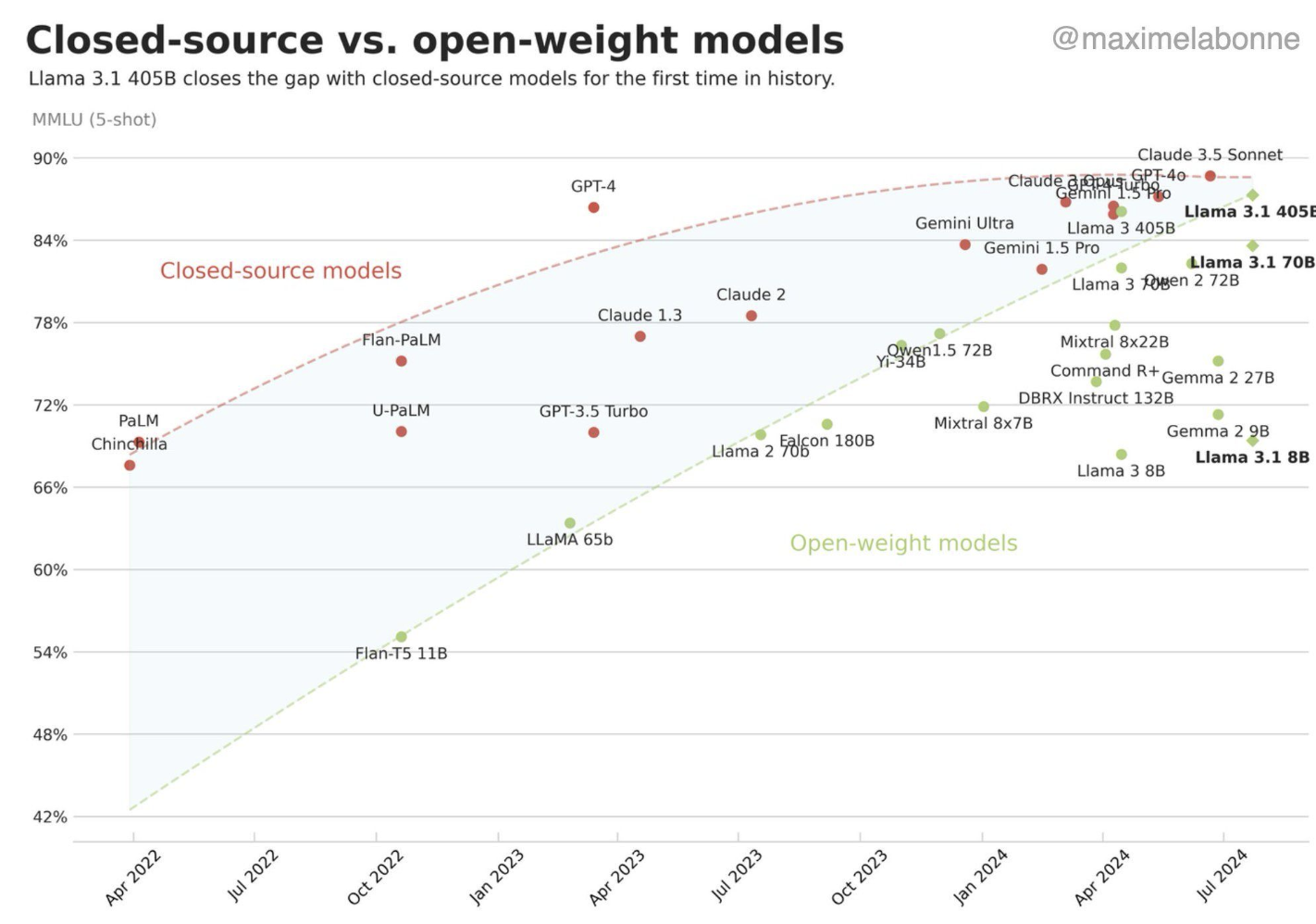
In recent years, the rapid evolution of artificial intelligence and the growing availability of digital medical data have positioned AI and machine learning as a promising solution. These technologies have shown promising results in mammography, in some studies, matching or even exceeding radiologists’ performance in breast cancer detection tasks. Research published in The Lancet Oncology revealed that AI-supported mammogram screening detected 20% more cancers compared to readings by radiologists alone. However, to achieve high accuracy, AI and ML models require training on large-scale, well-annotated mammography datasets.
The quality and inclusiveness of annotation directly influence model performance. Advanced annotation methods include diverse categorizations, such as lesion-specific labels, BI-RADS scores (Breast Imaging Reporting and Data System), breast density classes, and molecular subtype information. These annotated lesion datasets train the model to identify subtle imaging features that distinguish normal tissue from benign and malignant lesions, ultimately improving both sensitivity and specificity.
Breast cancer is a highly heterogeneous disease, displaying complexity at clinical, histopathological, microenvironmental, and genetic levels. Patients with different pathological and molecular subtypes show wide variations in recurrence risk, treatment response, and prognosis. This complexity must be reflected in training data if AI systems are to be clinically useful.
This write-up focuses on the importance of annotated data for building AI-powered models for lesion detection and how Cogito Tech’s Medical AI Innovation Hubs provide clinically validated, regulatory-compliant annotation solutions to accelerate AI readiness in breast cancer diagnostics.
Role of Annotated Datasets in Breast Cancer Detection
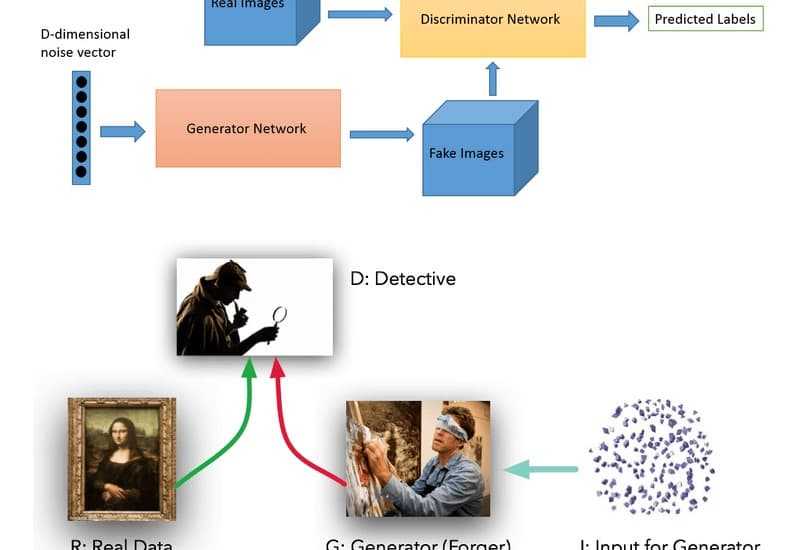
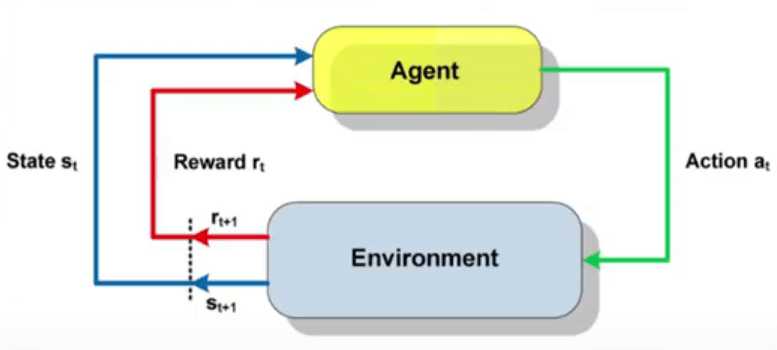
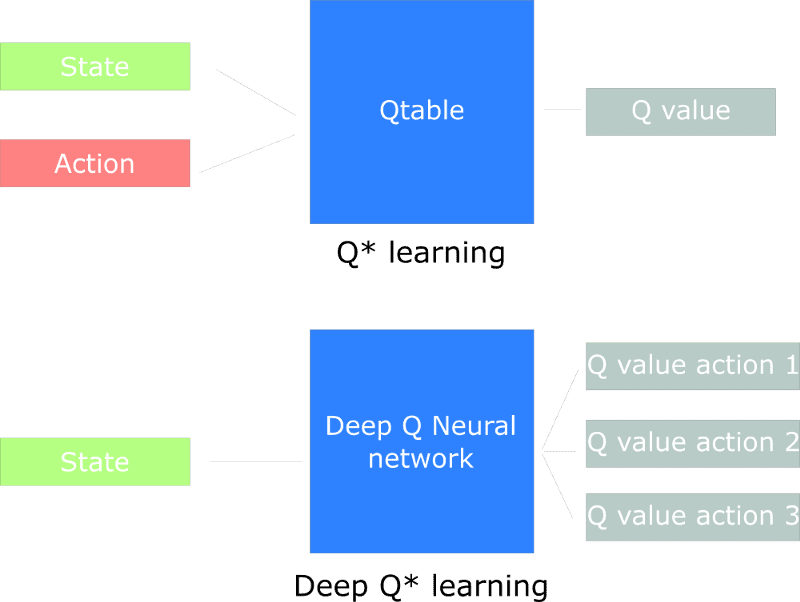
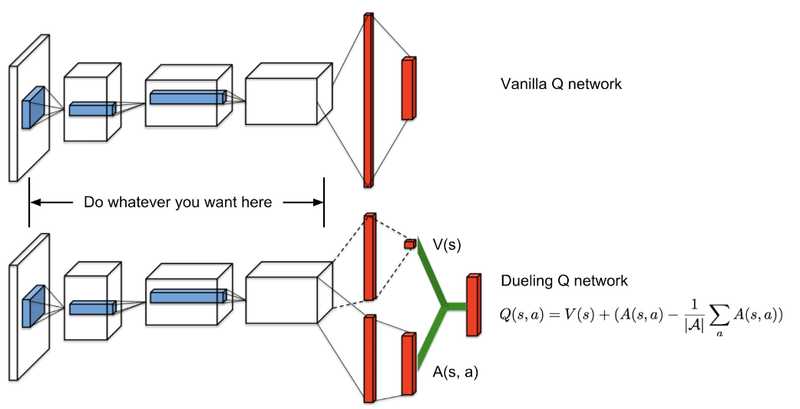
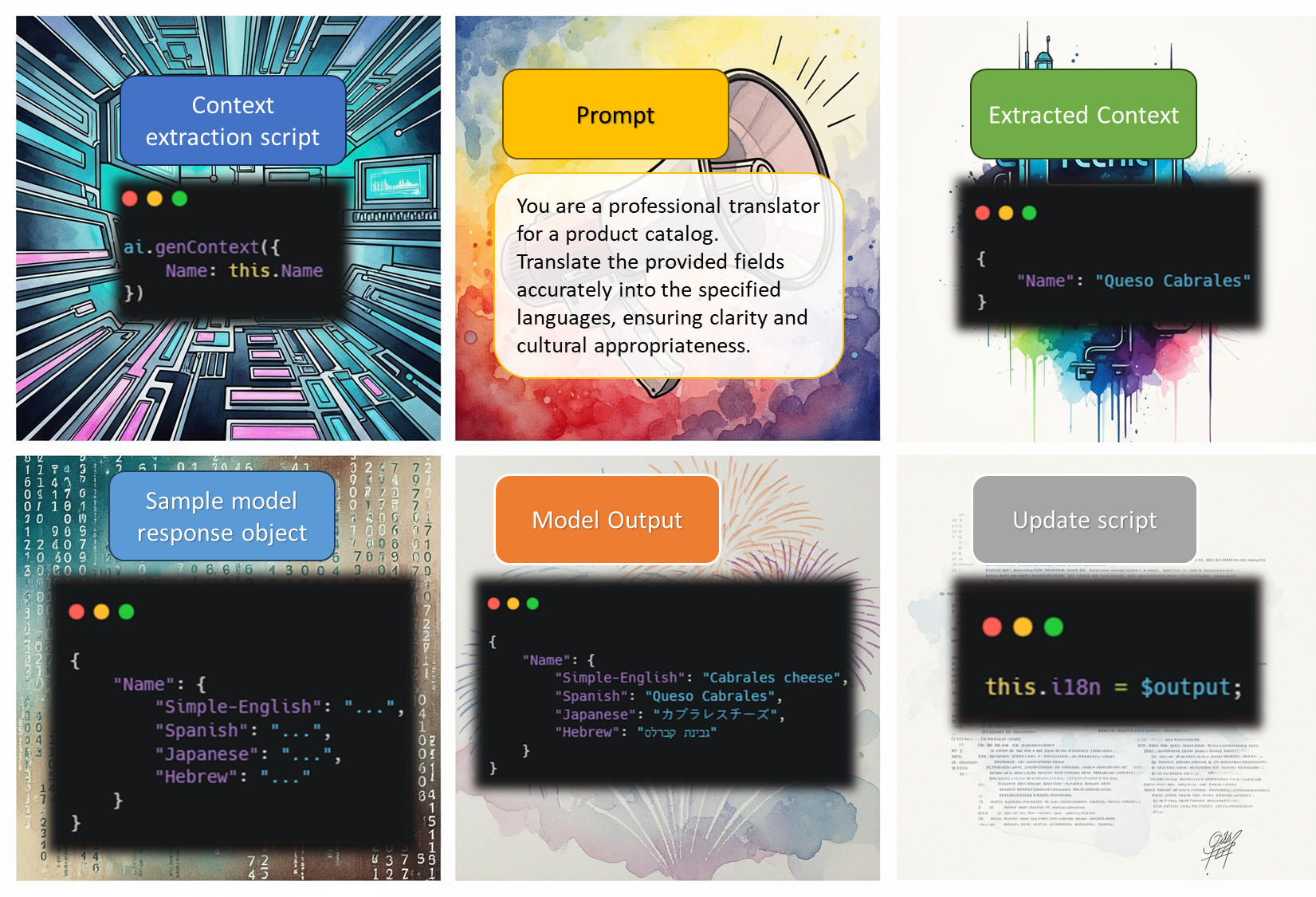
Medical data annotation serves as the fundamental infrastructure for training AI models in disease detection. In mammography, annotators, under the supervision of expert radiologists, mark lesions to create the ground truth labels necessary for supervised learning algorithms to analyze the complex patterns associated with different types of breast abnormalities. They apply bounding boxes, segment masks, and keypoints around suspicious areas on screening images. These labels guide neural networks, allowing the model to align its algorithm with the human-provided lesion annotations. Researches prove that deep learning models perform significantly better when trained with solid supervision—especially pixel-level annotations—compared to using only weak, image-level labels.
Large-scale, comprehensive datasets also enable models to generalize across diverse ethnic groups, age ranges, clinical workflows, and imaging data protocols, thereby mitigating the risk of overfitting to specific acquisition parameters (e.g., contrast, resolution, angle) and demographic characteristics.
Types of Mammography Data and Metadata
Training datasets that combine multiple types of breast imaging and associated clinical metadata are essential for building accurate AI models for lesion identification. Digital mammography is the primary and most fundamental type of breast imaging data, typically consisting of two distinct 2D X-ray views per breast: craniocaudal (cc) and mediolateral oblique (MLO).
Digital Breast Tomosynthesis (DBT), a 3D “pseudo-CT” series of thin X-ray slices through the breast, enhances detection rates—especially in dense breasts containing a lot of glandular and fibrous tissue, where tumors are difficult to detect in 2D images. DBT also reduces false positives compared to standard 2D mammograms. Algorithms trained on annotated DBT data can extract details from multiple angles to detect subtle lesions hidden by overlapping tissue.
In addition to annotated imaging data, clinical metadata, including patient age, clinical history, prior biopsy or surgeries, imaging parameters, and even recorded breast density (BI-RADS category), plays a critical role. This contextual information provides the model with valuable clues that can significantly improve the interpretation of the images and the likelihood of a lesion being cancerous. Metadata, especially related to breast tissue density and heterogeneity (often reported using BI-RADS), makes AI systems smarter and more robust. This allows the AI to factor in individual patient characteristics, leading to more accurate and reliable diagnoses.
To be effective, mammography datasets must be large and diverse, covering a wide range of ages, ethnicities, and varied lesion types. If training datasets belong predominantly to a single patient segment, biases can creep in, causing the model to underperform on underrepresented populations. Annotated images from multiple centers and diverse patient groups enable AI models to generalize well across the full screening population.
Annotation Techniques for Lesion Labeling
Here are common annotation methods used in mammography lesion labeling:
- Bounding Boxes: Radiologists draw rectangles around each lesion in the image. Bounding boxes are suitable for object-detection models that learn to propose and classify candidate regions. These boxes guide the model in focusing on the relevant area. For example, in the CBIS-DDSM (Curated Breast Imaging Subset of DDSM) dataset, the rectangle around the lesion is drawn as closely and accurately as possible.
- Semantic Segmentation: This pixel-level annotation technique outlines the exact shape of the lesion, allowing models to segment lesion boundaries precisely. Semantic segmentation provides dense training signals, enabling tasks such as volume measurement and shape analysis. Several datasets, such as CBIS-DDSM and LIDC-IDRI (for lung nodules), include full lesion contours. Such dense annotations typically enhance model performance, as supervised learning with pixel-level masks generally outperforms coarse, image-level labels.
- Keypoints or Landmark Points: This technique involves placing a single point at the center or at a characteristic spot on the lesion. It is more common in 3D imaging. In mammography, keypoints may mark the tip of a spiculated lesion—often a strong indicator of malignancy—or highlight individual microcalcifications.
- Multi-label Classification: Other than single, precise annotations, images or ROIs are often tagged with multiple attributes. For example, an image may contain both a malignant mass and a benign calcification, each receiving its own label. Radiologists may also tag lesion subtype, margin characteristics, or the associated BI-RADS category. In the CBIS-DDSM dataset, each ROI is labeled as a “mass” or “calcification” and further classified as benign or malignant. Multi-label datasets allow a single image to train several related classifiers simultaneously.
Annotation Tools and Workflows
Annotating mammography data typically requires special tools for complex medical image formats (like DICOM) and workflows. When selecting a medical image annotation tool, consider the following factors.
- Annotation Capabilities in Medical Imaging Viewers: Ensure the tool supports DICOM, NIfTI, and other formats, and allow annotators to precisely draw ROIs, outline lesions on 2D slices or 3D volumes using pen, polygon, and brush tools, and create segmentation masks linked to image voxels. They should also enable synchronized viewing of different types of medical scans.
- Annotation Type: Select a tool that supports various annotation methods required for labeling mammogram images, such as bounding boxes, polygons, and segmentation.
- User Interface: The tool should have a user-friendly interface that is easy to use for radiologists and other annotators, and it must be compatible with healthcare workflows.
- Export Formats: Ensure that the tool can export annotations in formats compatible with common machine learning frameworks.
- Compliance: The tool must meet FDA, HIPAA, and EMA regulations at every step, ensuring the highest safety, privacy, and accuracy standards for medical data.
Challenges in AI-Powered Breast Cancer Diagnosis
One of the greatest challenges in implementing AI-based breast cancer diagnosis is standardization. Differences in imaging equipment, protocols, and patient demographics often lead to performance inconsistencies when AI systems are transferred across institutions. Technical variations in image resolution and preprocessing further hinder model generalization.
Currently, widely used datasets are often insufficient, sourced from only a small number of institutions, and tied to specific mammographic machine vendors—creating a risk of algorithmic overfitting.
How Cogito Tech Improves Mammography Lesion Detection
With over a decade of experience, Cogito Tech’s Medical AI Innovation Hubs combine medical professional-led data annotation, efficient workflow management, and strategic partnerships to provide high-quality, FDA-and-HIPAA-compliant labeling that boosts diagnostic accuracy and accelerates AI development timelines. Cogito Tech’s medical annotation enhances accuracy in mammography lesion detection through:
- Global Network of Medical Talent: Cogito Tech’s team of board-certified medical professionals, including radiologists, pathologists, and pulmonologists from hospital networks worldwide—benchmark and validate labeled data to train ML models to detect lesions, tumors, and other abnormalities in mammograms.
- Strategic Partnerships: By leveraging advanced tools from partners, including RedBrick AI, ENCORD, V7, and Slicer, Cogito Tech’s annotation workforce accurately localizes anomalous tissue on 2D and 3D mammograms. From pre-labeling to production, quality control, and auditing, our teams use sophisticated annotation tools to meet diverse project needs.
- Transparent and Compliant Framework: Leveraging DataSum, our “Nutrition Facts” style framework for AI training data, we improve transparency around data quality while ensuring compliance with CFR 21 Part 11 and simplifying FDA 510(k) clearances.
- Format-Agnostic Support: Cogito’s medical annotation workforce works with diverse medical data formats, including NRRD, NIFTI, and DICOM, to support radiology, pathology, and other medical AI applications.
By leveraging DataSum to implement unified standards for data normalization and annotation from collection to labeling, Cogito addresses the fundamental variability and fragmentation issues that hinder AI model performance in breast cancer diagnosis.
Conclusion
Data annotation for mammography lesion detection provides a critical foundation for developing effective AI-powered diagnostic systems that have the potential to transform breast cancer screening and detection. Comprehensive, high-quality annotation, sophisticated preprocessing pipelines, and specialized DICOM-compatible tools are essential for training robust and generalizable models. The impact of annotation quality on diagnostic accuracy is substantial, with accurately labeled datasets enabling lesion detection systems to achieve performance levels that match or surpass those of human radiologists in specific tasks.
However, realizing the full potential of AI in mammography requires more than just advanced algorithms. It also demands the acquisition of relevant data, rigorously annotated and demographically diverse datasets, along with careful attention to regulatory and ethical considerations.
Cogito Tech’s Medical AI Innovation Hubs play a pivotal role in this ecosystem by providing clinically validated, FDA- and HIPAA-compliant annotations through a global network of board-certified radiologists and medical experts. Recognizing breast cancer’s biological complexity and the technical variability in imaging environments, Cogito bridges the gap between high-quality annotation and clinical AI readiness by leveraging strategic partnerships with platforms like RedBrick AI, ENCORD, V7, and Slicer, as well as proprietary frameworks such as DataSum for transparency and regulatory compliance. This integrated approach accelerates development timelines, enhances diagnostic accuracy, and lays the foundation for scalable, trustworthy AI solutions in breast cancer care.
The post Mammogram Data Annotation for AI-Driven Breast Cancer Detection appeared first on Cogitotech.
















































































































































![[The AI Show Episode 156]: AI Answers - Data Privacy, AI Roadmaps, Regulated Industries, Selling AI to the C-Suite & Change Management](https://www.marketingaiinstitute.com/hubfs/ep%20156%20cover.png)
![[The AI Show Episode 155]: The New Jobs AI Will Create, Amazon CEO: AI Will Cut Jobs, Your Brain on ChatGPT, Possible OpenAI-Microsoft Breakup & Veo 3 IP Issues](https://www.marketingaiinstitute.com/hubfs/ep%20155%20cover.png)

























































































































































































































_incamerastock_Alamy.jpg?width=1280&auto=webp&quality=80&disable=upscale#)
_Brain_light_Alamy.jpg?width=1280&auto=webp&quality=80&disable=upscale#)






















































































![Senators reintroduce App Store bill to rein in ‘gatekeeper power in the app economy’ [U]](https://i0.wp.com/9to5mac.com/wp-content/uploads/sites/6/2025/06/app-store-senate.jpg?resize=1200%2C628&quality=82&strip=all&ssl=1)