AppealRX
Inspiration Mental health claims are denied at nearly twice the rate of other medical services. Solo practitioners—who represent 47% of psychologists—often lack the billing staff, legal teams, or infrastructure to effectively handle appeals. As a result, patients are left to navigate complex policy language and administrative processes on their own. We saw an opportunity to build a tool that empowers individuals to advocate for themselves with the support of AI, precedent, and payer-specific policy guidance. What it does AppealRX helps patients rewrite and improve insurance appeal letters after a denial of mental health services. Users upload their draft, doctor’s note, and any supporting documents. The system analyzes the submission, retrieves similar past appeals and policy rules, and returns a refined draft with specific suggestions. AppealRX also includes a success prediction model—a classifier trained on historical appeal outcomes—which scores each draft’s likelihood of being approved. Together, these tools give users both actionable edits and a clear understanding of how their case compares to successful ones. How we built it We built the frontend using TypeScript with Next.js. On the backend: MongoDB stores user drafts, model outputs, and metadata. Pinecone is used as our vector database, indexing past appeals, insurer policies, and mental health guidelines. A fine-tuned BERT model classifies whether a draft appeal is likely to result in a favorable decision. A custom Retrieval-Augmented Generation (RAG) pipeline retrieves relevant legal and clinical language, which is incorporated into our rewriting and suggestion engine. To manage vector scaling, we route queries by insurance provider and preprocess large PDFs (e.g., insurer policies) to extract and index only relevant content. Challenges we ran into The biggest challenge was data quality. Medical appeals data was often unstructured and inconsistent. Many documents included the appeal decision in the note body, introducing label leakage. We resolved this by applying lemmatization and filtering out any sentence containing outcome-related terms like "denied", "approved", or "overturned". We also had to manage the rapid growth of our vector database. As more appeals and documents were added, retrieval became slower. To address this, we built a routing layer that narrowed search scope based on the user’s insurer. This ensured fast and relevant responses. Finally, working with real policy documents meant preprocessing PDFs to extract key terms (e.g., definitions of medical necessity, exclusions for mental health treatment) and making them accessible to the RAG pipeline. Accomplishments that we're proud of Built a fully functioning RAG-based appeal assistant in under 36 hours. Fine-tuned a BERT classifier to predict appeal outcomes with strong accuracy. Designed a scalable retrieval system that adapts to user context (e.g., insurer). Created a clean and intuitive user interface that lowers the barrier to action for patients facing denials. What we learned We learned how important proper preprocessing is when working with real-world clinical data. We also gained experience in building scalable vector pipelines and routing logic to maintain speed and relevance. From a product perspective, we saw how underserved the space of patient advocacy is—especially in mental health. Many people simply do not appeal because the system is hard to understand and navigate. A small improvement in clarity can dramatically increase someone’s chance of getting the care they need. What's next for AppealRX We plan to: Expand beyond mental health to other types of medical denials (e.g., chronic conditions, surgery). Partner with advocacy nonprofits and solo practices to pilot real-world use. Add provider-facing tools that allow clinicians to auto-generate appeals on behalf of patients. Build dashboards to track common reasons for denial and recommend best practices for successful appeals. Ultimately, we aim to make the appeals process less opaque, more fair, and more accessible for everyone—starting with those who need it most. Github App

Inspiration
Mental health claims are denied at nearly twice the rate of other medical services. Solo practitioners—who represent 47% of psychologists—often lack the billing staff, legal teams, or infrastructure to effectively handle appeals. As a result, patients are left to navigate complex policy language and administrative processes on their own. We saw an opportunity to build a tool that empowers individuals to advocate for themselves with the support of AI, precedent, and payer-specific policy guidance.
What it does
AppealRX helps patients rewrite and improve insurance appeal letters after a denial of mental health services. Users upload their draft, doctor’s note, and any supporting documents. The system analyzes the submission, retrieves similar past appeals and policy rules, and returns a refined draft with specific suggestions.
AppealRX also includes a success prediction model—a classifier trained on historical appeal outcomes—which scores each draft’s likelihood of being approved. Together, these tools give users both actionable edits and a clear understanding of how their case compares to successful ones.
How we built it
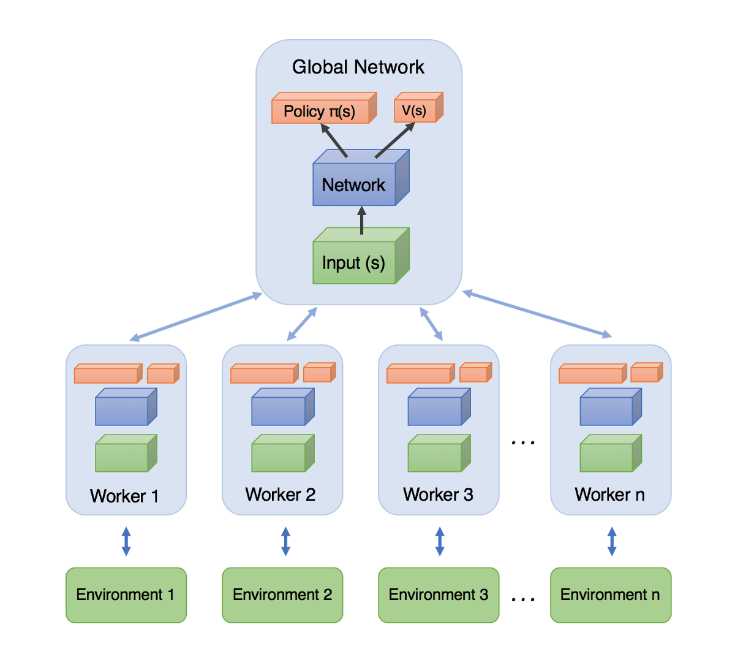
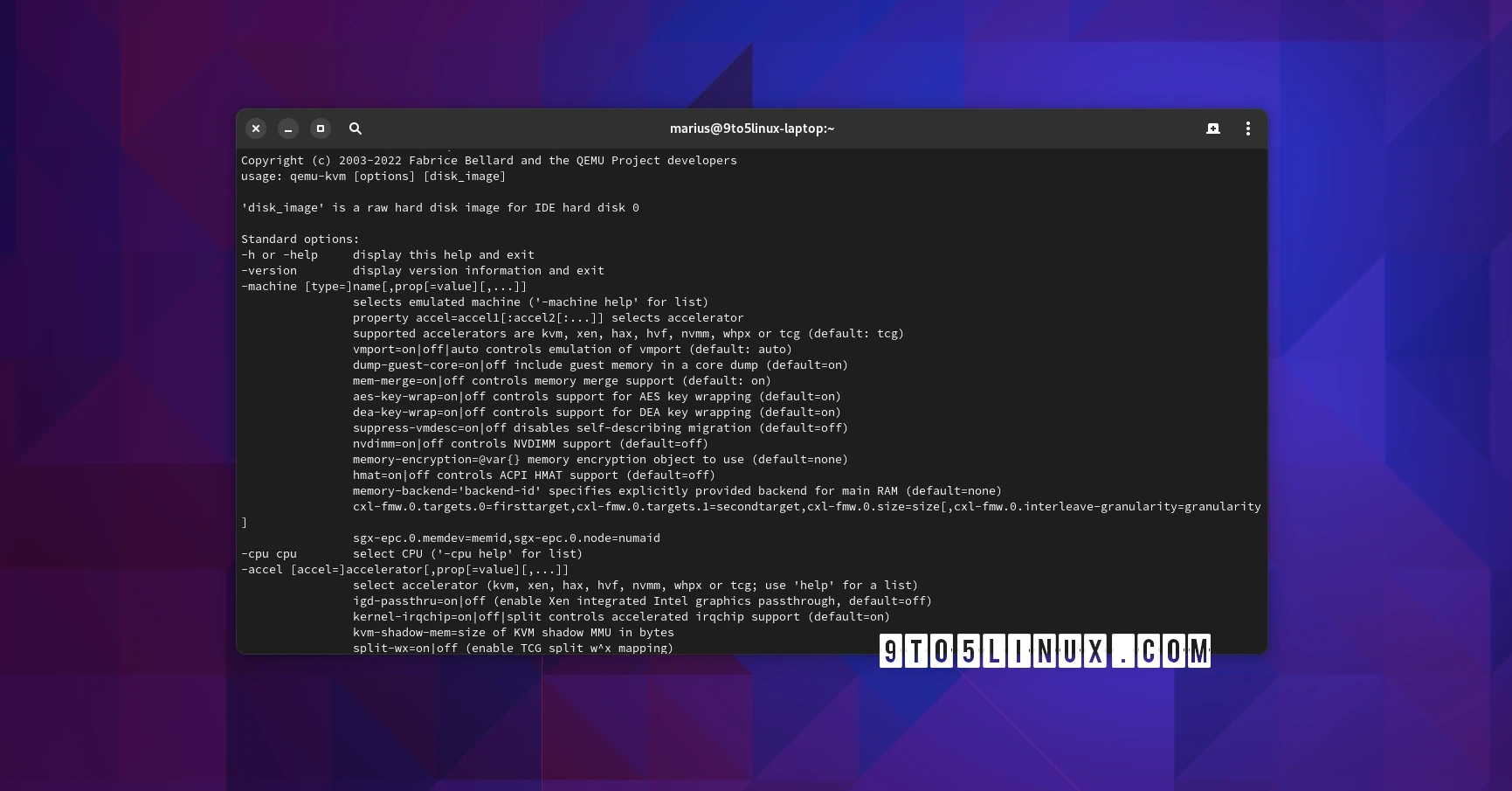
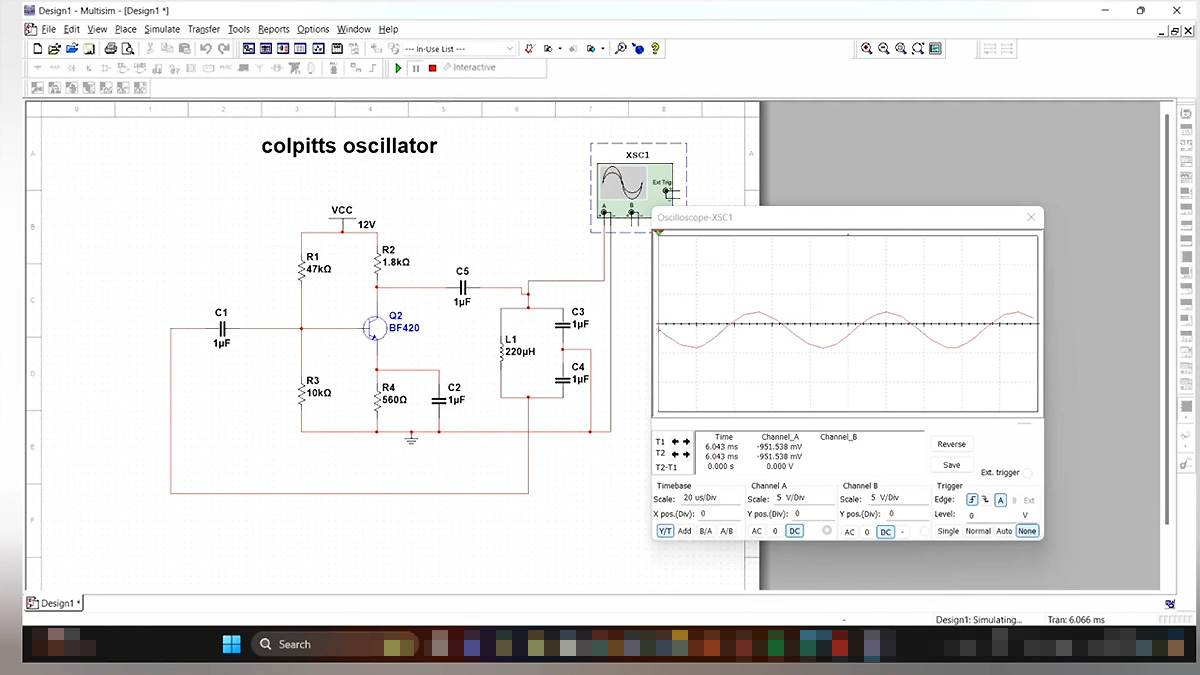
We built the frontend using TypeScript with Next.js.
On the backend:
MongoDB stores user drafts, model outputs, and metadata.
Pinecone is used as our vector database, indexing past appeals, insurer policies, and mental health guidelines.
A fine-tuned BERT model classifies whether a draft appeal is likely to result in a favorable decision.
A custom Retrieval-Augmented Generation (RAG) pipeline retrieves relevant legal and clinical language, which is incorporated into our rewriting and suggestion engine.
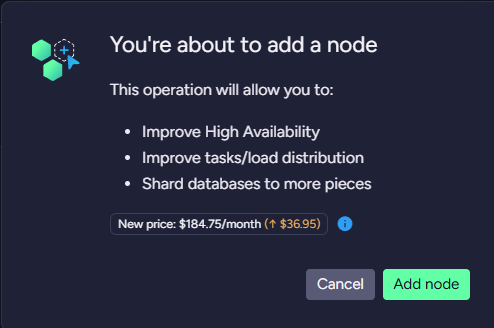
To manage vector scaling, we route queries by insurance provider and preprocess large PDFs (e.g., insurer policies) to extract and index only relevant content.
Challenges we ran into
The biggest challenge was data quality. Medical appeals data was often unstructured and inconsistent. Many documents included the appeal decision in the note body, introducing label leakage. We resolved this by applying lemmatization and filtering out any sentence containing outcome-related terms like "denied", "approved", or "overturned".
We also had to manage the rapid growth of our vector database. As more appeals and documents were added, retrieval became slower. To address this, we built a routing layer that narrowed search scope based on the user’s insurer. This ensured fast and relevant responses.
Finally, working with real policy documents meant preprocessing PDFs to extract key terms (e.g., definitions of medical necessity, exclusions for mental health treatment) and making them accessible to the RAG pipeline.
Accomplishments that we're proud of
Built a fully functioning RAG-based appeal assistant in under 36 hours.
Fine-tuned a BERT classifier to predict appeal outcomes with strong accuracy.
Designed a scalable retrieval system that adapts to user context (e.g., insurer).
Created a clean and intuitive user interface that lowers the barrier to action for patients facing denials.
What we learned
We learned how important proper preprocessing is when working with real-world clinical data. We also gained experience in building scalable vector pipelines and routing logic to maintain speed and relevance.
From a product perspective, we saw how underserved the space of patient advocacy is—especially in mental health. Many people simply do not appeal because the system is hard to understand and navigate. A small improvement in clarity can dramatically increase someone’s chance of getting the care they need.
What's next for AppealRX
We plan to:
Expand beyond mental health to other types of medical denials (e.g., chronic conditions, surgery).
Partner with advocacy nonprofits and solo practices to pilot real-world use.
Add provider-facing tools that allow clinicians to auto-generate appeals on behalf of patients.
Build dashboards to track common reasons for denial and recommend best practices for successful appeals.
Ultimately, we aim to make the appeals process less opaque, more fair, and more accessible for everyone—starting with those who need it most.

















































































































































![[The AI Show Episode 144]: ChatGPT’s New Memory, Shopify CEO’s Leaked “AI First” Memo, Google Cloud Next Releases, o3 and o4-mini Coming Soon & Llama 4’s Rocky Launch](https://www.marketingaiinstitute.com/hubfs/ep%20144%20cover.png)






























































































































































































-All-will-be-revealed-00-35-05.png?width=1920&height=1920&fit=bounds&quality=70&format=jpg&auto=webp#)











































































































![What iPhone 17 model are you most excited to see? [Poll]](https://9to5mac.com/wp-content/uploads/sites/6/2025/04/iphone-17-pro-sky-blue.jpg?quality=82&strip=all&w=290&h=145&crop=1)
















![Hands-On With 'iPhone 17 Air' Dummy Reveals 'Scary Thin' Design [Video]](https://www.iclarified.com/images/news/97100/97100/97100-640.jpg)
![Mike Rockwell is Overhauling Siri's Leadership Team [Report]](https://www.iclarified.com/images/news/97096/97096/97096-640.jpg)
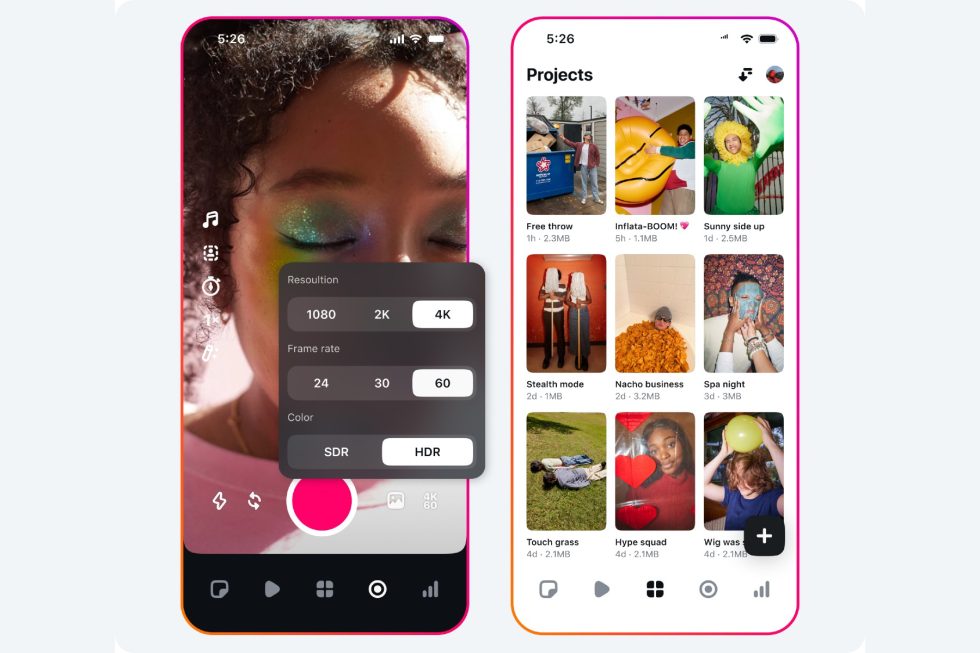
![Instagram Releases 'Edits' Video Creation App [Download]](https://www.iclarified.com/images/news/97097/97097/97097-640.jpg)
![Inside Netflix's Rebuild of the Amsterdam Apple Store for 'iHostage' [Video]](https://www.iclarified.com/images/news/97095/97095/97095-640.jpg)